Evidence-Based Healthcare Design
Aug - Dec 2019 | Productivity, Health, & the Sustainable Quality of the Built Environment | Advised by: Vivian Loftness and Suzy Li
The design of architecture can have a significant impact on the occupant’s health. This is especially true in healthcare design to help minimise the risk of nosocomial infections, infections that are acquired during a patient’s stay in the hospital. Nosocomial infections can be reduced in different ways or a combination of different ways. The following series of research provides three methods that have proven to drastically reduce patient’s risk of hospital-acquired infections (HAI).
By minimising the risk of nosocomial infections, there can be a reduced cost of special treatment against the infections, which in turn helps the hospitals save money from the operational costs of such treatments. Low nosocomial infection rate would also improve a hospital’s reputation as well as relations with medical insurance companies, both of which would help increase the number of patients. Furthermore, not only will patients be recovering in an environment with a lower risk of acquiring nosocomial infections, but also the medical staff will be working in an environment that is more safe for their health, and ultimately, the patients in need of their care.
Use of HEPA filters
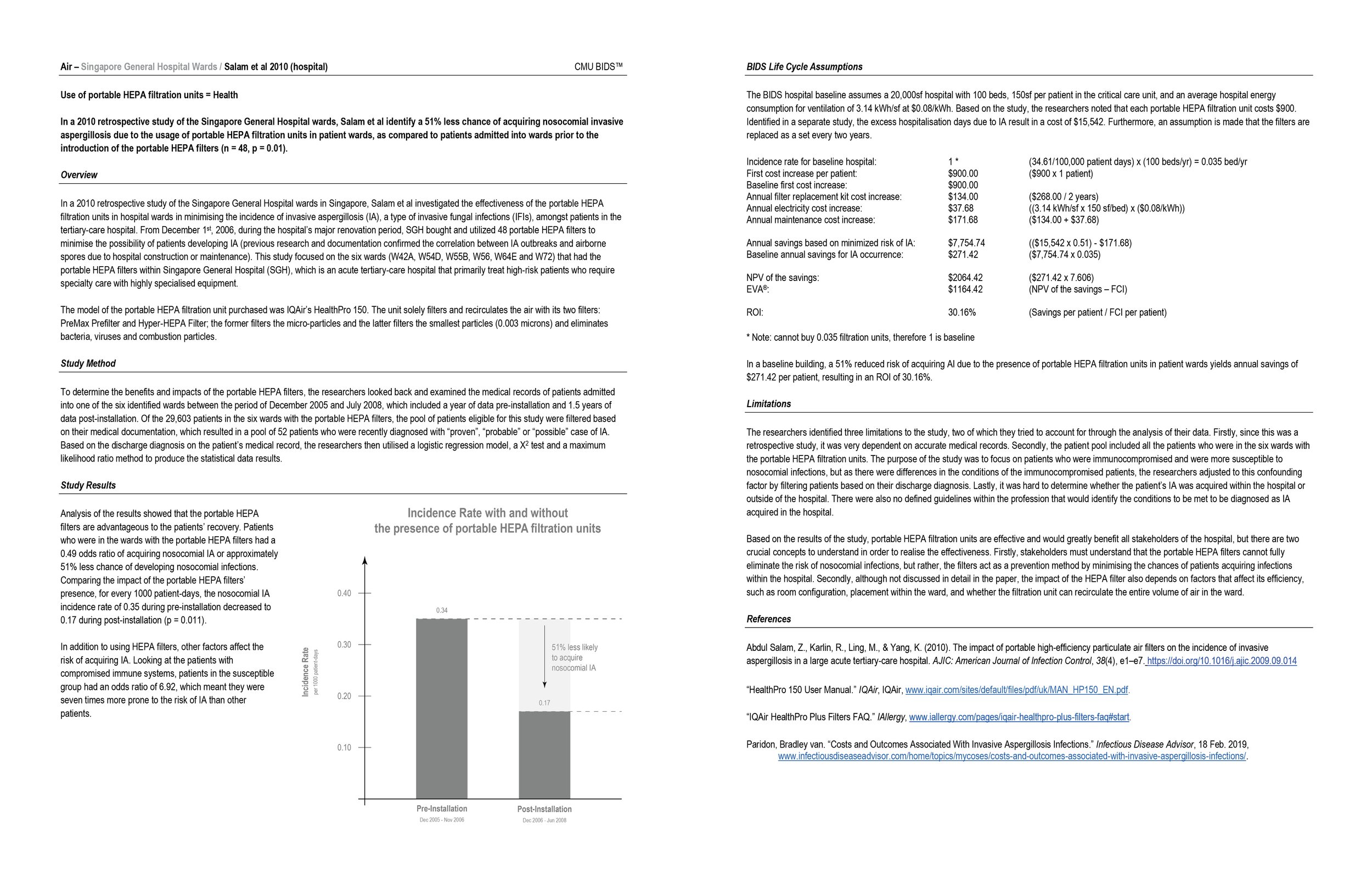
Salam et al. conducted a retrospective study of the Singapore General Hospital wards to investigate the effectiveness of the portable HEPA filtration units in minimising the incidence of invasive aspergillosis (IA) and identified a 51% less chance of acquiring nosocomial IA (n = 48, p = 0.01).
Improve natural ventilation to increase air changes/hour
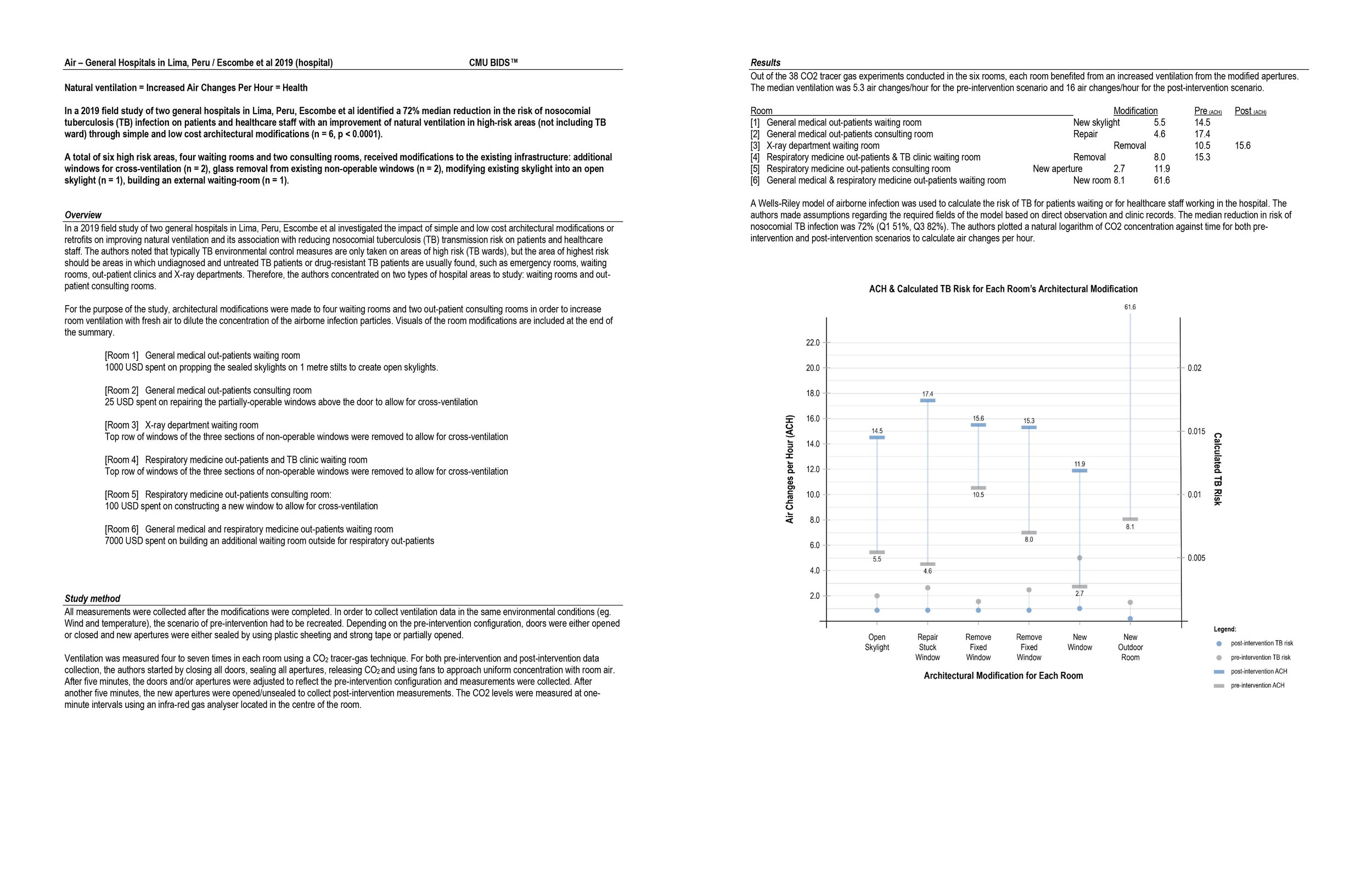
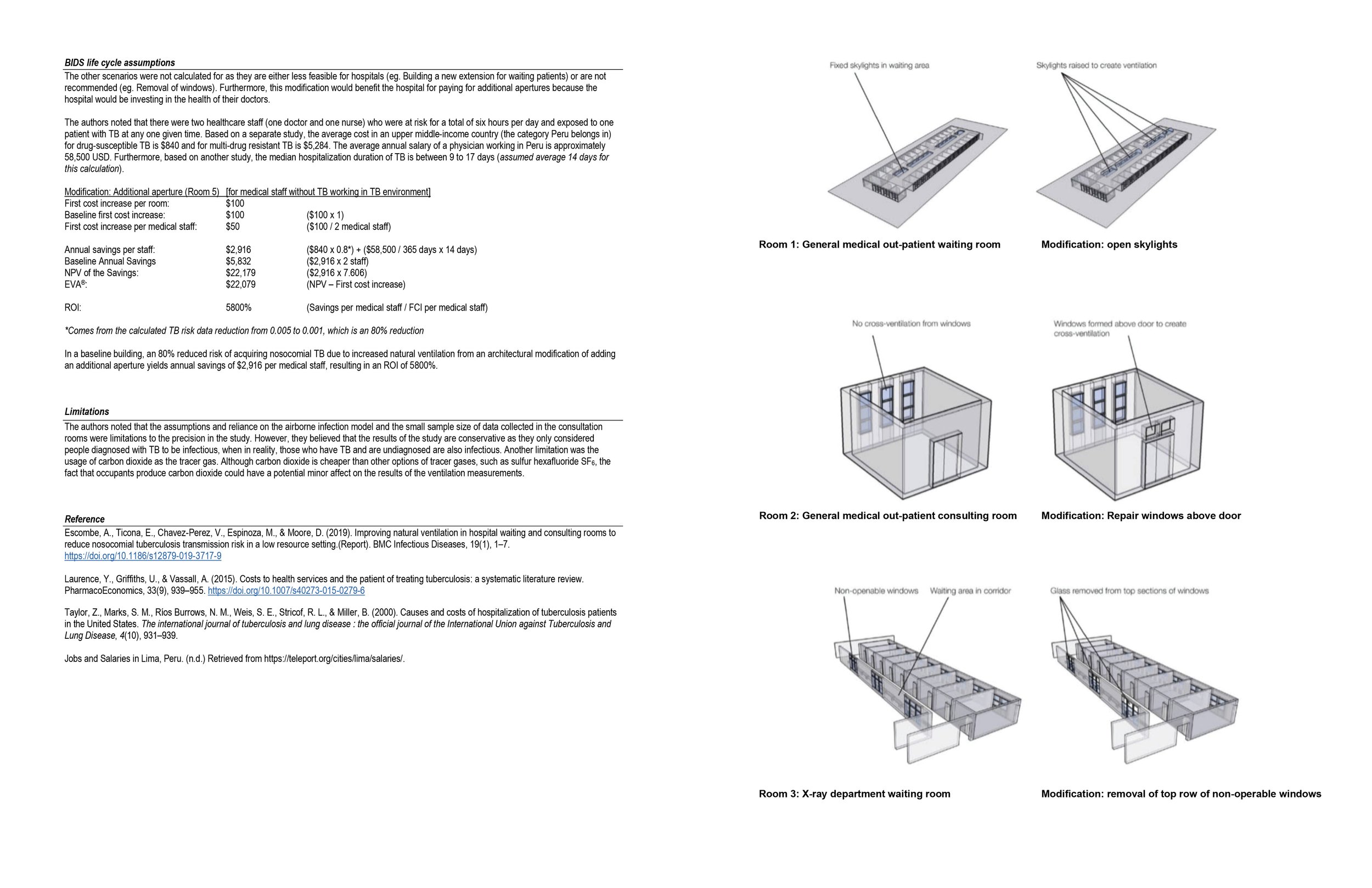
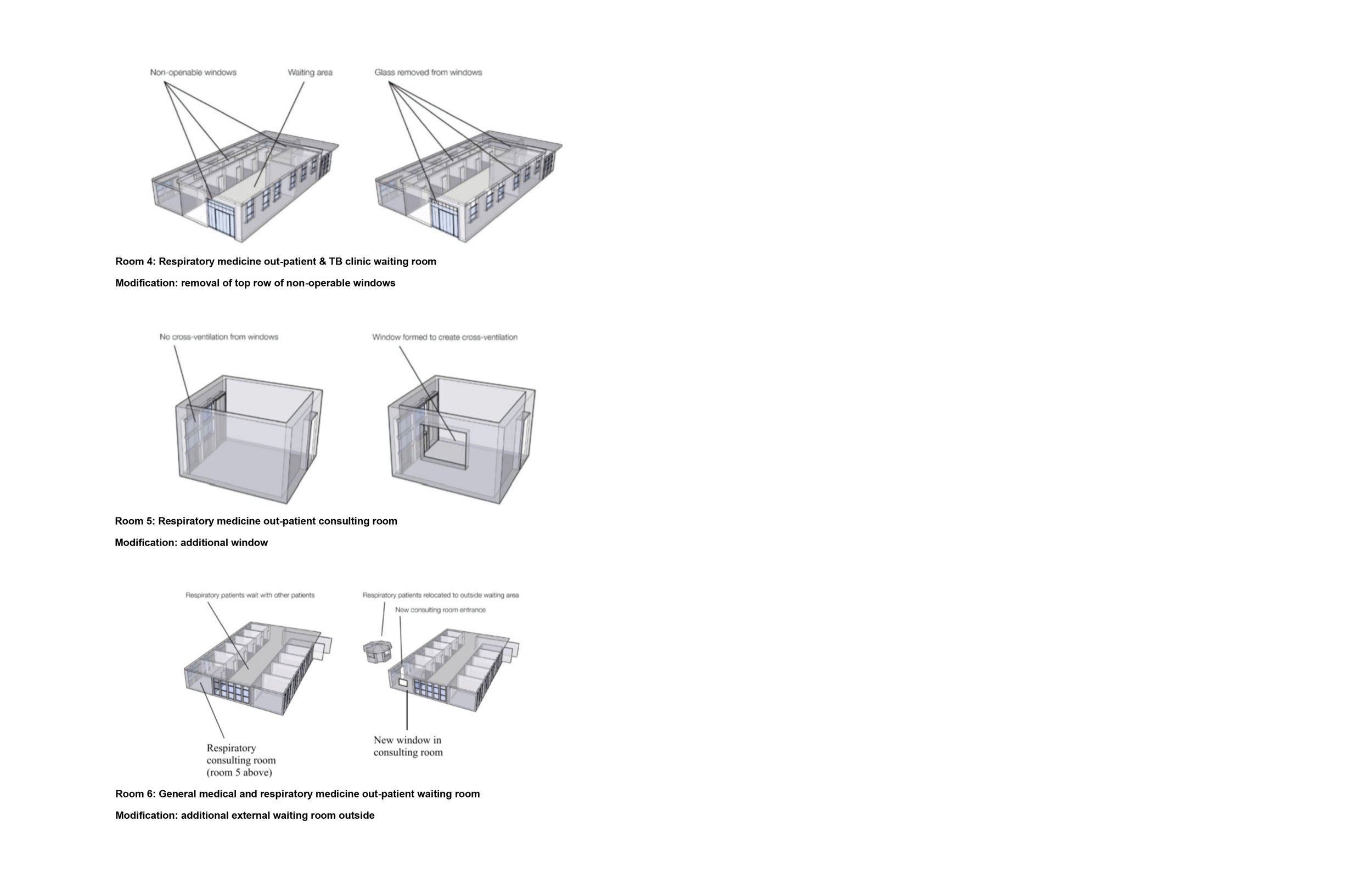
Escombe et al. conducted a field study of two general hospitals in Lima, Peru to investigate the impact of simple and low-cost architectural modifications or retrofits on improving natural ventilation and its association with reducing nosocomial tuberculosis (TB) transmission risk on patients and healthcare staff. The authors identified an 80% reduction in the risk of acquiring nosocomial TB due to increased natural ventilation and air changes per hour (ACH) from an architectural modification of adding an additional aperture (n = 6, p < 0.0001).
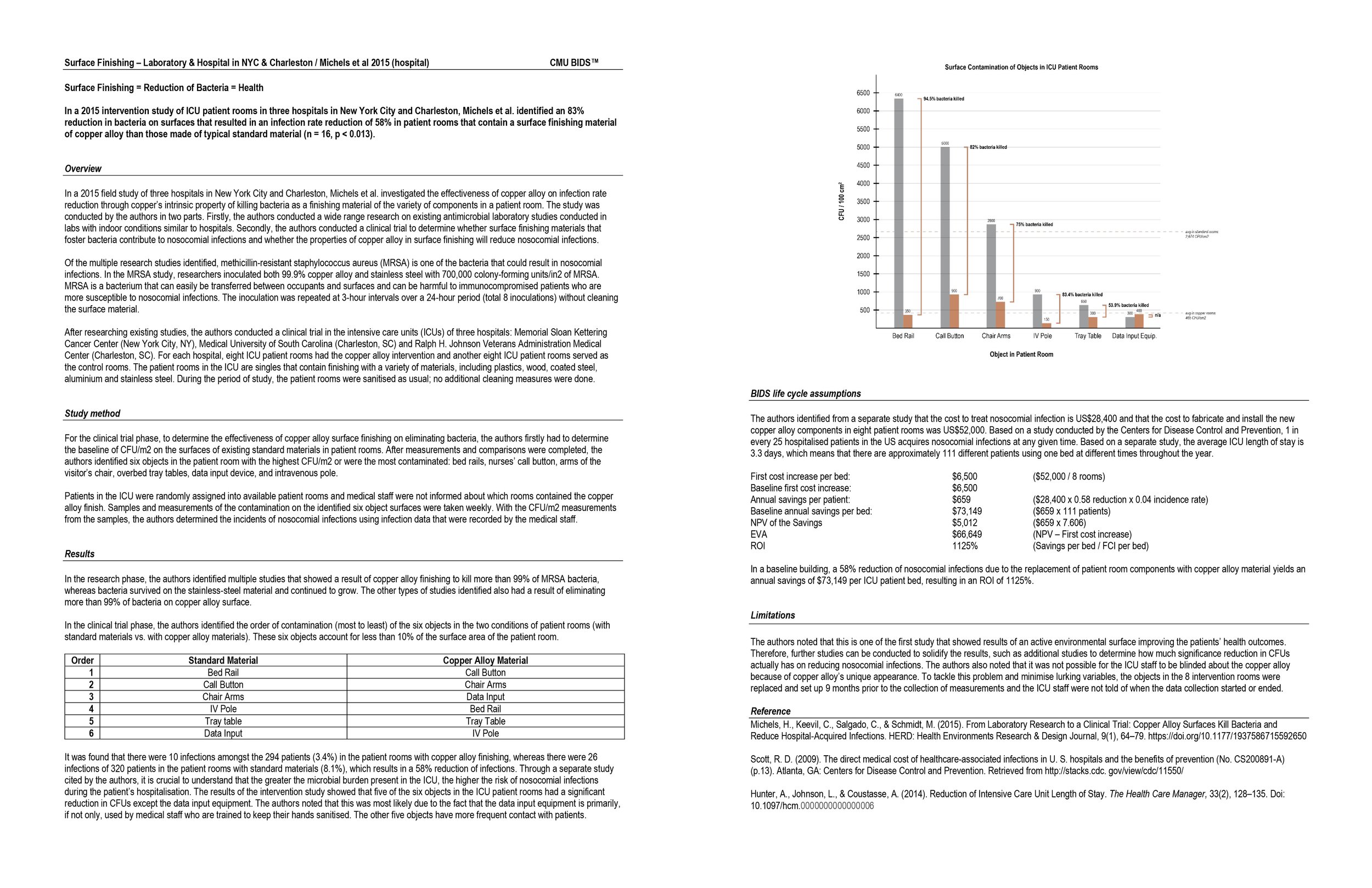
Replacement of standard materials with copper alloy
Michels et al. conducted an intervention study of ICU patient rooms in three hospitals in New York City and Charleston to investigate the effectiveness of copper alloy on infection rate reduction (copper has an intrinsic property of killing bacteria) as a finishing material of the variety of components in the patient room. The six components tested were objects that are frequently in contact with patients and healthcare staff: bed rail, call button, chair arms, IV pole, tray table, data input equipment. The authors identified an 83% reduction of bacteria on copper alloy finishing components that resulted in a 58% reduction of nosocomial infections (n = 16, p = 0.013).